Abstract
Purpose/Objective(s): Radiation therapy (RT) plays an important role in treating Solitary Extramedullary (EMP) and Solitary Bone (SBP) Plasmacytomas. The objective of this study is to review the effectiveness of RT in locally controlling the disease and looking at factors that predict progression to Multiple Myeloma (MM) in the PET scan-era.
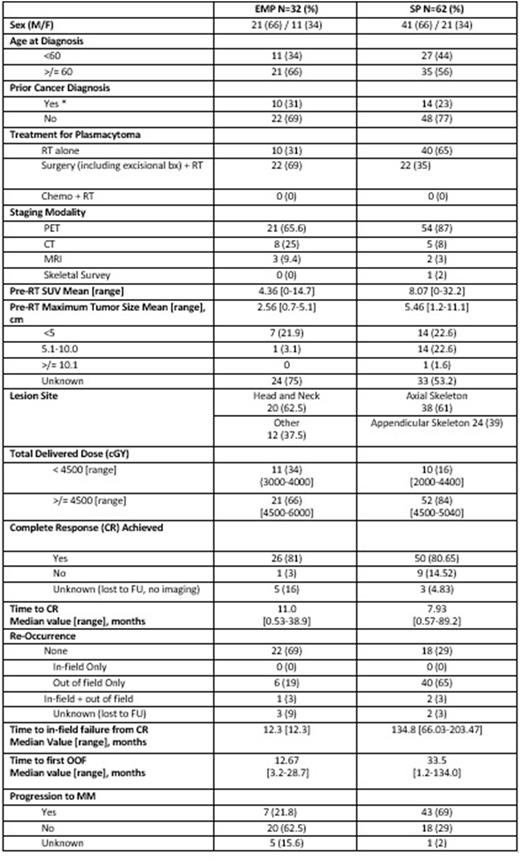
Materials/Methods: We performed a retrospective analysis of consecutive plasmacytoma patients (pts) treated at our high-volume center. We identified 94 pts, of which 62 were diagnosed with SBP and 32 with EMP, without evidence of MM at diagnosis (end-organ damage, >10% bone marrow involvement, >1 plasmacytoma). We identified 94 total pts, largest series to date in the literature, treated with RT (no pts received systemic therapy) between January 1, 2000, through December 31, 2020. Of the 94 pts, 62 were diagnosed with SBP and 32 with EMP, without evidence of MM at diagnosis (end-organ damage, >10% bone marrow involvement, >1 plasmacytoma). We utilized radiographic staging including PET scans and clinical assessments to determine patient outcomes. Outcomes include initial radiographic responses using the European Expert Panel Response Criteria, local control (LC), overall survival (OS), and progression to MM. Kaplan-Meier was used to assess LC and OS. Univariable analysis was done using age, sex, race, plasmacytoma type (EMP vs. SBP), PET scan at staging versus other modalities, first post-RT response (CR, no CR), Pre-RT SUV of lesion, RT dose (≥45Gy) and overall response to RT (if CR was achieved).
Results: Patient and treatment characteristics are summarized in table 1. 24 (66%) EMPs and 54 (84%) SBPs received a radiation dose ≥45Gy. After excluding 8 patients who were lost to follow up, 81% of patients with EMPs and 81% with SBPs achieved complete response (CR) with a median time to CR being 11 months (range 0.53-38.9) for EMP and 8 months (range 0.6-89.2) for SBP. All pts achieving a CR were treated with doses ≥40Gy. Only 1 (3%) EMP and 2 (3%) SBPs had an in-field failure after CR. The 5-year OS was 68% for EMPs and 94% for SBPs [p=0.007]. Out of 94 pts, 19 died, and cause of death was not related to the plasma cell neoplasm in 7 EMP pts. The 5-year rate of progression to MM was 28% in the EMP group, and 64% in the SBP group [p=0.006], with progression-free survival (PFS) of 61% In the EMP group and 35% in the SBP group [p=0.041]. On univariate analysis, sex, age, RT dose (<45 Gy, ≥45 Gy), staging PET, location [EMP vs. SBP] and achieving a CR after RT (at first post-RT response and CR at any time) were analyzed. Pts with EMP were at significantly lower risk for progression to MM (HR 0.3, 95% CI 0.2, 0.8; p=0.009) Additionally, Pts with CR on first post-RT imaging were at lower risk for progression to MM (HR 0.6, 95% CI 0.3, 1.0, p=0.05).
Conclusion: Our data indicates that definitive RT for EMP and SBP can provide excellent LC. Progression to MM remains the main problem and is more common among pts with SBP, which is concordant with previously published literature.
Disclosures
Imber:GT Medical Technologies: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal